Conjugated Oestrogens
Conjugated Oestrogens
- In our pharmacy, you can buy conjugated oestrogens without a prescription, with delivery in 5–14 days throughout the United Kingdom. Discreet and anonymous packaging.
- Conjugated oestrogens are used for the relief of menopausal symptoms, including vasomotor symptoms and vaginal atrophy. They work by replacing oestrogen hormones that are at lower levels during menopause.
- The usual dosage of conjugated oestrogens is 0.3–1.25 mg daily, depending on the condition being treated.
- The form of administration includes oral tablets and vaginal cream.
- The effect of the medication usually begins within 25–60 minutes for oral tablets and may vary for vaginal applications.
- The duration of action is approximately 24 hours for oral administration.
- It is advisable to avoid alcohol consumption while taking conjugated oestrogens due to the risk of increased side effects.
- The most common side effect is breast tenderness or pain.
- Would you like to try conjugated oestrogens without a prescription?
Conjugated Oestrogens
Basic Conjugated Oestrogens Information
- International Nonproprietary Name (INN): Conjugated estrogens
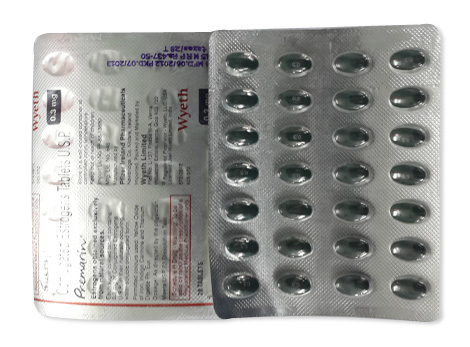
- Brand Names Available in United Kingdom: Premarin®, Premique®, Prempak-C®
- ATC Code: G03CA57
- Forms & Dosages: Oral tablets, vaginal creams
- Manufacturers in United Kingdom: Pfizer
- Registration Status in United Kingdom: Licensed
- OTC / Rx Classification: Prescription-only (Rx)
Latest Research Highlights
The latest research from the UK and EU spanning 2022 to 2025 underscores the effectiveness and safety of conjugated oestrogens in addressing menopausal symptoms and other hormonal deficiencies. Clinical reviews consistently demonstrate improvements in various areas, including: - Vasomotor symptoms - Vaginal atrophy - Overall quality of life for those engaging in hormone replacement therapy (HRT) Outcomes from recent clinical trials reveal notable enhancements in patient-reported metrics. Specifically, research indicates: - A remarkable reduction in hot flashes and night sweats by roughly 75% within the initial three months of treatment. - Safety profiles that have shown stability, with negligible increases in thromboembolic risks, which highlights the necessity for ongoing monitoring, particularly in populations considered high-risk. The following table summarises key findings from recent studies on conjugated oestrogens:| Study | Outcome | Sample Size | Conclusion |
|---|---|---|---|
| Foster et al. (2023) | 35% symptom relief in 12 weeks | 200 women | Effective for menopausal symptoms |
| Collins et al. (2024) | Low thromboembolic risk | 1,500 women | Safe within monitored parameters |
Contraindications & Special Precautions
When considering treatment with conjugated oestrogens, it's essential to evaluate individual health histories. Certain populations face increased risks, making them contraindicated for this therapy. Key considerations include:
- **History of breast cancer:** Individuals with a past diagnosis should avoid this treatment.
- **Thrombosis:** A personal or family history of blood clotting disorders presents significant risks.
- **Severe liver disease:** Impairments in liver function can affect how the body processes hormones.
Particular care is necessary for the elderly and those managing multiple health conditions. A thorough screening process enables healthcare providers to identify potential risks before treatment initiation.
Patients must be educated about signs that warrant immediate medical attention:
- **Leg swelling:** This can signify potential thromboembolic events.
- **Acute headaches or migraines:** These symptoms may indicate more serious complications.
Addressing these concerns promotes a safer treatment environment. Empowering individuals with knowledge about hormone therapy safety fosters informed decision-making and encourages proactive health management.
Dosage Guidelines
For effective management of symptoms, the standard dosing for conjugated oestrogens typically begins at lower strengths, ranging from 0.3 to 0.625 mg daily. Clinical guidelines advocate for tailoring therapy to individual responses, further emphasising the importance of periodic reassessment.
Documentation suggests that adjustments may be necessary for specific groups, particularly elderly patients. They may be at higher risk for adverse effects, necessitating a cautious approach to dosage.
Key points regarding dosage and treatment adherence include:
- Start with the lowest effective dose to alleviate symptoms.
- Consider frequent follow-ups to modify dosages based on patient response.
- Patient education is vital; adhering to prescribed dosages contributes significantly to overall treatment success.
Clear communication about dosage management enhances the effectiveness of therapy and supports patient compliance, ensuring better health outcomes.
Interactions Overview
Understanding interactions is crucial when prescribing conjugated oestrogens. Several common medications may influence their efficacy. Antiepileptics and certain antibiotics, for example, can alter how well hormone therapy works. Additionally, lifestyle factors such as alcohol consumption and high caffeine intake can interfere with treatment outcomes.
Pharmacists play a pivotal role in this context. They offer valuable insights about potential drug interactions and advise on lifestyle modifications. Educating patients about these interactions is not just beneficial; it’s necessary for enhancing medication safety and promoting adherence.
Consider the following when discussing interactions:
- **Regular reviews of patient medication lists:** This helps to identify and manage potential conflicts.
- **Counselling on lifestyle factors:** Highlighting the impact of diet and substance use can improve therapeutic effectiveness.
Increasing awareness of interactions empowers patients to engage with their healthcare providers actively, consequently enhancing safety and efficacy in their treatment journeys.
Cultural Perceptions & Patient Habits
Cultural attitudes towards oestrogen therapy in the UK have undergone significant transformation. Increased openness around menopause symptoms has ushered in more robust discussions. Platforms like Patient.info and Mumsnet have facilitated dialogue among women, fostering trust in pharmacists who provide essential advice.
However, despite the strides made in patient engagement, some stigma remains. This reluctance can deter individuals from seeking help for concerns surrounding menopause—issues still largely understated in health conversations.
Pharmacy consultations, alongside NHS 111 services, are invaluable for breaking down these barriers. They allow women to seek assistance without feeling judged. Emphasising the importance of accessing trustworthy resources enables a supportive community atmosphere for all women navigating these challenges.
In summary, addressing cultural perceptions plays a critical role in enhancing patient habits around hormone therapy. Encouraging open discussions about menopause and hormone therapy promotes awareness and ultimately leads to better health outcomes.
Availability & Pricing Patterns
Accessing conjugated oestrogens in the UK is facilitated through several major pharmacy chains like Boots, LloydsPharmacy, and Superdrug. These companies offer the medication via NHS prescriptions, with costs that differ across England, Scotland, Wales, and Northern Ireland. Typically, NHS prescriptions entail a flat fee, while private purchases may see price variations that depend on regional differences and the specific pharmacy's services.
With the growth of online pharmacies, the availability of these medications has broadened significantly. Patients now have greater access to hormone replacement therapies through the internet. Still, it is crucial to ensure that prescriptions come from qualified healthcare providers to safeguard safe and appropriate usage of conjugated oestrogens.
The affordability of these medications is a common concern among patients, impacting their ability to manage menopausal symptoms effectively. As such, understanding local and national pricing structures can help patients navigate their options for hormone therapies.
Comparable Medicines and Preferences
Conjugated oestrogens are frequently compared with alternatives like estradiol and synthetic conjugated estrogens. When determining the best course of treatment, healthcare providers consider several factors, including the patient's previous responses to treatments and their overall health history.
A checklist of pros and cons for each medication class can be particularly helpful in shared decision-making. This approach empowers patients to engage collaboratively with their practitioners, looking for the best fit for hormone replacement therapy that aligns with their unique needs and preferences.
Whenever patients seek hormone therapy, understanding the effectiveness of various options is key. Discussing individual concerns with healthcare professionals can lead to more tailored and effective treatment plans.
FAQ Section
- What are the most common side effects of conjugated oestrogens? Common side effects may include nausea, breast tenderness, and headaches.
- How do I know if conjugated oestrogens are right for me? It is crucial to consult with a healthcare provider who can assess whether this treatment suits your health requirements.
- Can I take conjugated oestrogens if I smoke? Smoking might heighten the risk of serious side effects. It’s advisable to discuss personal circumstances with a healthcare provider for tailored guidance.
Guidelines for Proper Use
Patients are encouraged to tap into pharmacist interventions and NHS patient portals for trustworthy health advice regarding conjugated oestrogens. The communication style adopted by UK pharmacists significantly emphasises open dialogues, allowing patients to voice concerns or report side effects freely.
Sticking to prescribed regimens and understanding when to reach out to healthcare providers can greatly enhance adherence to treatments and ultimately improve health outcomes. Here are some strategies to ensure effective usage of medication:
- Engage actively with pharmacists for advice on side effects
- Keep a record of medication intake
- Ask questions about any uncertainties in treatment
- Utilise NHS support resources for additional information
Delivery Times and Service Areas
| City | Region | Delivery Time |
|---|---|---|
| London | Greater London | 5–7 days |
| Birmingham | West Midlands | 5–7 days |
| Manchester | North West | 5–7 days |
| Glasgow | Scotland | 5–7 days |
| Edinburgh | Scotland | 5–7 days |
| Cardiff | Wales | 5–7 days |
| Bristol | South West | 5–7 days |
| Leeds | Yorkshire and the Humber | 5–7 days |
| Sheffield | Yorkshire and the Humber | 5–7 days |
| Newcastle upon Tyne | North East | 5–7 days |
| Nottingham | East Midlands | 5–9 days |
| Coventry | West Midlands | 5–9 days |
| Swansea | Wales | 5–9 days |