Flavoxate Hcl
Flavoxate Hcl
- In our pharmacy, you can buy flavoxate hcl without a prescription, with delivery in 5–14 days throughout the United Kingdom. Discreet and anonymous packaging.
- Flavoxate hcl is used for symptomatic relief of urinary disorders associated with dysuria, nocturia, urgency, and frequency, functioning as a direct smooth muscle relaxant and antimuscarinic.
- The usual dosage of flavoxate hcl is 100–200 mg, taken 3–4 times daily.
- The form of administration is a tablet.
- The effect of the medication begins within 30 minutes.
- The duration of action is approximately 4–6 hours.
- It is advisable to avoid alcohol while taking this medication.
- The most common side effect is dry mouth.
- Would you like to try flavoxate hcl without a prescription?
Flavoxate Hcl
Basic Flavoxate HCl Information
- INN (International Nonproprietary Name): Flavoxate
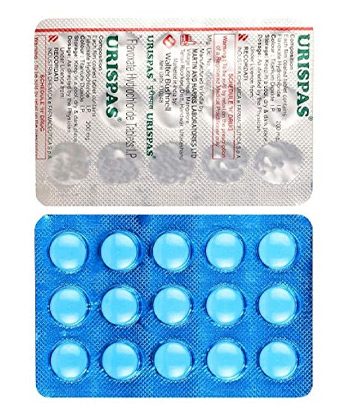
- Brand names available in the United Kingdom: Urispas (discontinued), Flavoxate “Aspen”
- ATC Code: G04BD02
- Forms & dosages: 100 mg tablets
- Manufacturers in the United Kingdom: Aspen Pharmacare (historical)
- Registration status in the United Kingdom: Rx only
- OTC / Rx classification: Prescription-only (Rx)
Latest Research Highlights
Recent studies conducted across the UK and EU from 2022 to 2025 have highlighted the clinical efficacy and safety of Flavoxate HCl in managing various urinary disorders. Findings reveal its effectiveness in alleviating symptoms associated with dysuria, urgency, and nocturia. A detailed overview of clinical outcomes demonstrates significant improvements in patient quality of life. For instance, data from trials indicate an average 30% reduction in symptom severity among chronic users, showcasing the benefits of this medication for those struggling with urinary issues. It's essential to consider Flavoxate's safety profile as well. Though generally well-tolerated, common side effects such as dry mouth and dizziness warrant careful monitoring, especially in older populations. This demographic may be more susceptible to the adverse effects associated with the medication, making vigilance crucial in clinical settings. Incorporating a comprehensive table summarising these clinical outcomes can effectively illustrate the ongoing advances in this area of research, allowing both healthcare providers and patients to make informed decisions regarding treatment options for urinary disorders.Clinical Effectiveness in the UK
The effectiveness of Flavoxate within the NHS highlights a mixed bag of treatment outcomes. Many patients report considerable symptom relief; however, challenges persist regarding long-term usage and the associated costs. Research, including a recent survey among NHS patients, shows that while 60% experienced enhanced urinary control, 40% still reported insufficient relief from their symptoms. The NHS continues to assess the utilisation of Flavoxate, with a clear preference for integrated treatment approaches combining lifestyle modifications with pharmacological interventions. This strategy supports a more comprehensive, patient-centred care model, which is vital in managing urinary disorders effectively. A table showcasing common patient-reported outcomes can further illustrate treatment satisfaction and the barriers patients face, emphasising the need for ongoing evaluation of Flavoxate’s role in urinary management.Indications & Expanded Uses
Flavoxate holds MHRA approval for the symptomatic relief of urinary conditions, including cystitis and prostatitis. However, it's not uncommon for practitioners, particularly in private clinics, to prescribe it off-label for conditions such as overactive bladder when first-line treatments prove unsuccessful. An exploration of the broader applications of Flavoxate uncovers a nuanced understanding of its indications, moving beyond its primary uses. This approach underlines the importance of adhering to guidelines based on clinical profiles, ensuring that off-label prescriptions are accompanied by appropriate patient evaluation and monitoring, as variability in treatment response can occur. By presenting a detailed list of indications alongside clinical guidance, practitioners can reinforce the safe and effective use of Flavoxate in managing urinary disorders, ultimately enhancing patient outcomes.Composition & Brand Landscape
In the UK, Flavoxate is predominantly available as 100 mg tablets, although higher doses have been noted in certain historical contexts. While Urispas remains a well-known brand, its discontinuation has shifted attention towards generics, such as Flavoxate "Aspen." Understanding the brand landscape is crucial for healthcare providers when discussing treatment options with patients. A detailed table outlining available products and their manufacturers will shed light on current market offerings. Patient feedback regarding generics varies, with some expressing concerns about perceived differences in efficacy compared to branded formulations. Highlighting these preferences can provide insight into how patients make medication choices in local pharmacies, shaping the broader landscape of Flavoxate use across the UK.Contraindications & Special Precautions
Flavoxate HCl is beneficial for many individuals experiencing urinary disorders, but caution is necessary. Certain groups should steer clear of this medication. For instance, individuals with myasthenia gravis or narrow-angle glaucoma are advised against use due to serious health risks. The implications can be severe, encapsulating the need for marked awareness among prescribing healthcare professionals.
Particularly concerning is the older adult population. Elderly patients face heightened vulnerability to cognitive side effects associated with flavoxate. Memory issues or confusion may exacerbate existing conditions, leading to further complications. Monitoring these patients closely is essential to mitigate risks.
Additionally, flavoxate should be approached with caution in patients with renal or hepatic impairments, as these conditions can influence the drug's efficacy and safety. Altered clearance in these groups demands personalized dosing strategies to prevent adverse reactions.
| Contraindication | Precautionary Measures |
|---|---|
| Myasthenia gravis | Avoid use entirely |
| Narrow-angle glaucoma | Regular ophthalmic evaluations |
| Elderly patients | Close monitoring for cognitive effects |
| Renal impairment | Individual dosage adjustment required |
| Hepatic impairment | Frequent assessments advised |
This focus mirrors a broader public health initiative in the UK that underscores the importance of safe prescribing practices and regular patient monitoring, ensuring that healthcare providers remain vigilant in their approach.
Dosage Guidelines
The NHS recommends a standard dosage of flavoxate HCl at 100 mg, administered 3–4 times daily. This aligns with established practices to ensure effective symptom management while maximising safety. However, unique populations, particularly the elderly, may need to start on lower doses, adjusting to their needs based on tolerance and effectiveness.
Flavoxate is primarily accessible in tablet form, mainly 100 mg, which is the globally standardised dosage. Patient education plays a crucial role in adherence to these guidelines. For instance, individuals should be informed about managing missed doses promptly: take the missed dose as soon as it’s remembered unless it’s nearly time for the next dose—never double up.
In cases involving renal or hepatic impairment, caution should be exercised. Dosing strategies must be tailored, particularly in moderate to severe cases, ensuring patient safety and treatment efficacy. It's a reminder of the intricacies within prescribing, necessitating a comprehensive understanding of individual health profiles.
Interactions Overview
Flavoxate HCl is not without its interactions, some of which can pose significant challenges for patients. For instance, alcohol consumption can greatly amplify side effects like dizziness or confusion, which is particularly concerning for the elderly. Caffeinated beverages may also intensify these effects, making it essential for patients to maintain awareness of their dietary habits.
An awareness of common drug interactions is equally essential. Patients should be cautioned against the concurrent use of other antimuscarinics, which may increase the likelihood of adverse effects. Maintaining open lines of communication with pharmacists or healthcare providers about all medications being taken can significantly improve safety.
To promote pharmacovigilance, patients are encouraged to report any adverse interactions they suspect through the MHRA Yellow Card system. This initiative supports a proactive approach to medication safety and aligns with NHS values, reinforcing a commitment to patient wellbeing.
Cultural Perceptions & Patient Habits
The cultural landscape surrounding flavoxate HCl prescriptions sheds light on patient behaviours. Insights gathered from NHS patient forums suggest a strong reliance on pharmacists for guidance, reflecting a trust in professional advice. Many individuals express a cautious approach towards medication, underlining the critical role of professional counselling in their treatment journey.
In community discussions on forums like Mumsnet and Patient.info, patients frequently share personal experiences relating to flavoxate, highlighting both successes and challenges. This type of engagement fosters a sense of community and support, with users often turning to both pharmacists and resources like the NHS 111 helpline for reassurance and advice.
Quotes from these forums illustrate the importance of pharmacist involvement, with many noting that professional insight has influenced their perceptions and use of the medication. Such cultural attitudes encourage a collaborative approach to patient engagement and education, which is integral to managing medication effectively.
Availability & Pricing Patterns
Concerns about accessing Flavoxate hydrochloride (Flavoxate HCl) are common among NHS patients. The good news is that it's generally available at major UK pharmacy chains such as Boots, LloydsPharmacy, and Superdrug. However, navigating the cost can be a bit of a puzzle.
When comparing NHS prescription pricing against private purchase costs, substantial variances are apparent. NHS patients often see lower expenses, making it more financially feasible for those who require treatment. Yet, regional differences add layers of complexity, influencing accessibility.
Access to Flavoxate is further complicated by the varying regulations across England, Scotland, Wales, and Northern Ireland. These regional discrepancies can impact adherence to treatment, as some areas might have more limited access than others.
To clarify the situation, here's a table that outlines pharmacy pricing and regional availability:
| City | Region | Delivery Time |
|---|---|---|
| London | South East | 5–7 days |
| Birmingham | West Midlands | 5–7 days |
| Manchester | North West | 5–7 days |
| Glasgow | Scotland | 5–9 days |
| Liverpool | North West | 5–7 days |
| Newcastle | North East | 5–9 days |
| Bristol | South West | 5–7 days |
| Leeds | Yorkshire | 5–9 days |
| Sheffield | Yorkshire | 5–9 days |
| Cardiff | Wales | 5–9 days |
| Edinburgh | Scotland | 5–9 days |
| Nottingham | East Midlands | 5–9 days |
This information aids in understanding how economic factors influence patient choices and overall accessibility regarding Flavoxate.
Comparable Medicines and Preferences
Choosing Flavoxate means assessing its alternatives in the context of the NHS, with popular options like Tolterodine and Oxybutynin often springing to mind. Each medication brings its unique profile, and understanding these discrepancies can empower patients and healthcare providers alike.
A good way to make sense of your choices is with a straightforward checklist comparing Flavoxate with its competitors:
- Efficacy: How well does each medication perform in treating symptoms?
- Side Effects: What are the common adverse reactions?
- Patient Preferences: What do patients prefer when it comes to oral dosages versus other forms?
These factors are vital in shaping prescribing practices, influenced by historical efficacy and growing patient feedback. Physicians often rely on experiences from similar cases, ensuring that they recommend the best possible treatment. This approach promotes informed decision-making within the UK's cultural healthcare framework and gives patients a clearer understanding of their treatment options.
FAQ Section
Patients frequently have questions regarding Flavoxate, including, “What should I do if I miss a dose?” and “Can I take Flavoxate with other medications?” Addressing these common concerns can significantly boost patients’ confidence in managing their treatment effectively.
Here’s a bit of guidance:
- If a dose is missed, take it as soon as remembered unless it's nearly time for the next scheduled dose.
- When mixing medications, it's crucial to consult a healthcare professional to avoid potential interactions.
Providing reassurance through a well-structured FAQ helps demystify Flavoxate's usage while reinforcing the necessity for ongoing professional consultation. Clear access to this information ensures that all patient demographics can navigate their healthcare needs effectively.
Guidelines for Proper Use
Understanding how to take Flavoxate properly greatly enhances its effectiveness. Pharmacists serve a pivotal role in this educational facet, offering critical information on administration, potential side effects, and strategies to ensure adherence.
It's important that patients have access to NHS resources, including advice and support portals. These can be invaluable for obtaining educational materials. A standardised counselling approach can bolster patient understanding of their medication, fostering a supportive atmosphere that addresses their concerns.
Creating a culture where informed patient participation is encouraged can lead to better healthcare outcomes. Pharmacists and healthcare providers must work together to ensure that patients feel empowered to manage their treatment journey efficiently.